You notify ThrivePass via our portal or electronic file, triggering a COBRA notice to the Qualified Beneficiary (QB). They can easily review and manage their options as all elections and payments can be handled online. If you're a COBRA Decision Enablement client, they'll also review alternative plan options and be recommended the best available plan for them —whether that's through COBRA or the federal and state Marketplaces.
We support state rules where they apply and federal rules everywhere else.
To simplify matters, we accept payments via direct debit (ACH) and credit card. Additionally, we highlight upcoming payment due dates or any declined payment attempts, ensuring it's easy to manage payments and avoid disruption of COBRA coverage.
Whether it's a severance and tipped employee program, LOA, or retired benefits, we'll work with you to build a program that best fits your needs and provides a streamlined experience for both you and the retiree.

On average, COBRA participants cost employer’s plans $10,000 per year and COBRA coverage costs participants around 27% more than plans available through the federal and state Marketplaces.
That's where ThrivePass's COBRA Decision Enablement comes in. Decision Enablement recommends the best available plan for participants —whether that's through COBRA or the federal and state Marketplaces.
Recommendations are based on the total cost of all possible plans for the participant, including premiums and out-of-pocket expenses. Oftentimes, that's not the COBRA plan.



With hundreds of federal and state Marketplace plans to choose from, Qualified Beneficiaries (QBs) can usually find a better alternative to COBRA. After answering a series of questions about their health and finances, QBs find the most affordable plan tailored to their needs.
When employees transition away from their current employment, they receive COBRA packets that direct them to COBRA Decision Enablement.
Qualified Beneficiaries (QBs) answer a series of questions before viewing available COBRA options. These questions help us recommend the most affordable alternative plan options based on their specific need.
With our recommendations and COBRA plans side-by-side, QBs can compare plans in real time, highlighting the cost differences and empowering them to make an informed choice.
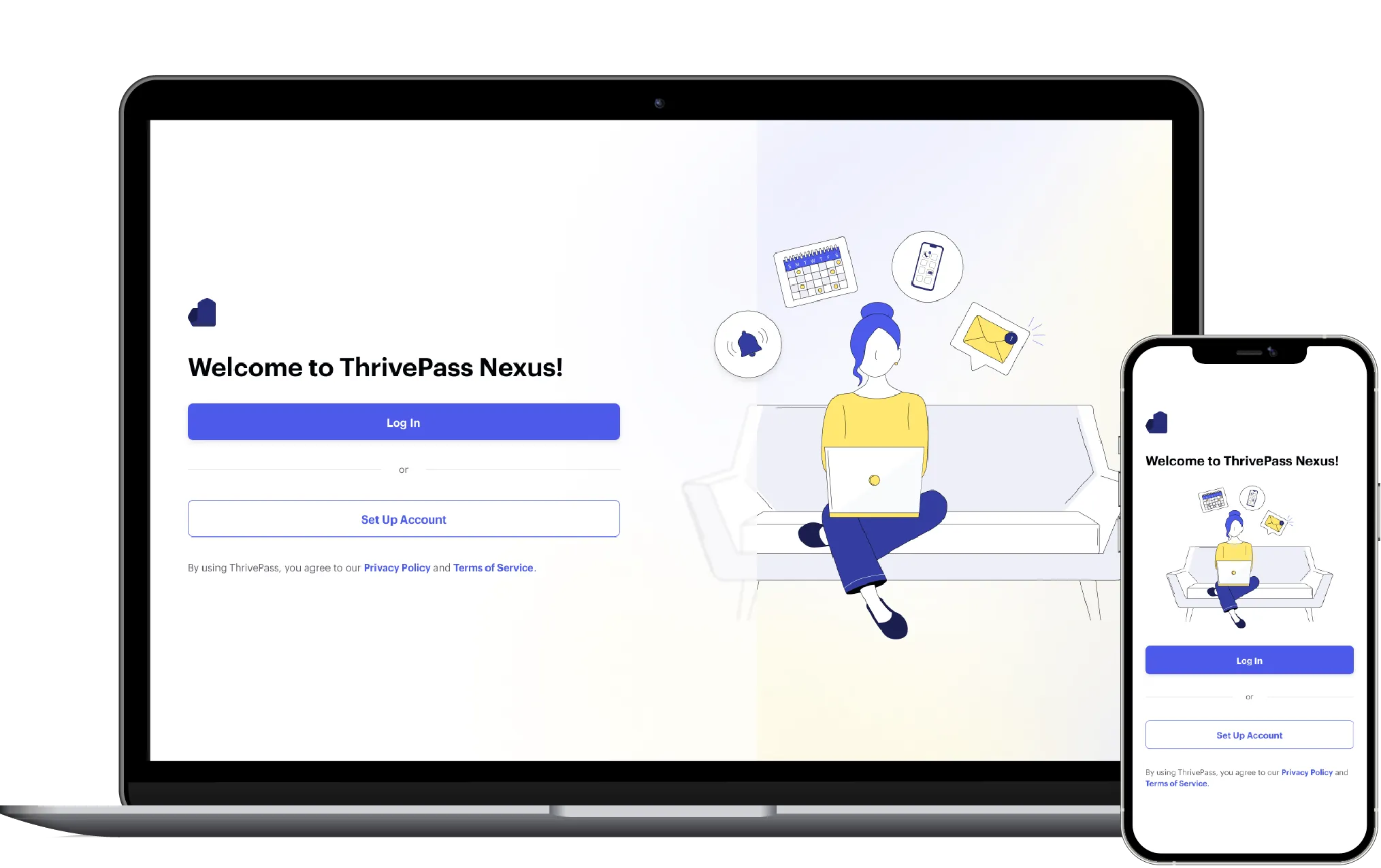
QBs then have the choice to move forward with COBRA elections or submit an application for the Marketplace plan. The entire experience, regardless of choice, can be handled easily online in a matter of a few minutes.